Mandated Benefits
New York currently mandates more than 55 specific benefits and services including:
- Asthma inhalers without cost sharing
- Autism spectrum disorder treatment
- Biomarker testing
- Bone mineral density measurements or tests, drugs, and devices
- Cervical cytology screening
- Chest wall reconstruction
- Chiropractic care
- Contraceptive drugs and devices
- Diabetic equipment, supplies, and self-management education
- Donor human breast milk
- Emergency services
- Enteral formulas
- Epi-pens with cost sharing cap
- Essential health benefits (Affordable Care Act)
- Experimental or investigational services recommended by an external appeal agent
- Eye drop refills
- Home health care
- Infertility treatment
- Infertility treatments regardless of sexual orientation or gender identity.
- Insulin without cost-sharing
- In-vitro fertilization (IVF) and fertility preservation services.
- Lung cancer follow up screening and diagnostic services
- Mammography screening
- Mastectomy care
- Maternity care
- Medical conditions leading to infertility
- Medication for the detoxification or maintenance treatment of a substance use disorder
- Mental health care services – inpatient
- Mental health care services – outpatient
- Neuropsychological exams for dyslexia
- Off label cancer drugs
- Orally administered anticancer medications
- Ostomy equipment and supplies
- Out-of-network dialysis
- Post-mastectomy reconstruction
- Pre- and post-natal care without cost sharing
- Pre-admission testing
- Pre-hospital emergency medical services
- Prenatal vitamins
- Preventive and primary health services
- Prostate cancer screening
- Scalp cooling caps for cancer patients
- Second medical opinion for cancer diagnosis
- Second surgical opinion
- Substance use services – inpatient
- Substance use services – outpatient
- Tattooing related to breast cancer reconstruction surgery
- Transvaginal ultrasound coverage
“Make Available”
- Ambulatory care
- Dependent coverage through age 29
- Hospice care
- Nursing home care
- Out-of-network benefits
- Registered nurse
- Social worker
- Supplemental home care
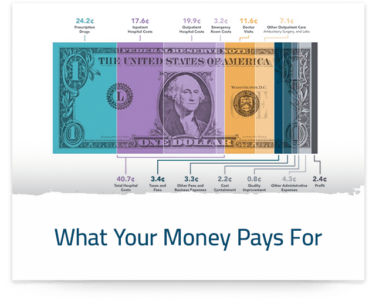
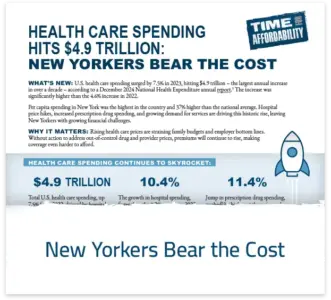
While the cost of individual mandates may be small, collectively they increase health insurance premiums and make coverage more expensive for employers and consumers.