MEMORANDUM IN OPPOSITION
FOR IMMEDIATE RELEASE: MAY 13, 2019
Re: S.3526 (Breslin)/A.6211 (Magnarelli) – AN ACT to amend the insurance law, in relation to payments to prehospital emergency medical services providers.
This legislation, S.3526/A.6211, would require health plans to directly reimburse ambulance service
providers regardless of whether they are in-network or out-of-network providers. The New York Health Plan Association (HPA) opposes this bill as it undermines the value of plan networks and would result in higher prices for ambulance services, leading to increased health insurance costs for consumers and employers.
Integrated health care networks are the foundation of health care plans. State law requires the
Department of Health to review and approve the adequacy of plans’ provider networks. Providing
coverage through a network increases quality, enhances medical competency and encourages greater
coordination and collaboration by providers. Networks also promote cost efficiencies, which help make health care more affordable and accessible. Building a quality network requires considerable skill and a menu of incentives that encourage providers to join a network.
Health plan networks are organized to provide members with a broad list of providers from which they can seek care, at a predetermined rate billed directly to and paid by the health plan. Providers join networks because they provide a new pool of potential patients and the direct financial relationship with the plan ensures providers benefit from a complete and timely payment of claims, improved cash flow and certainty in budgeting. There are already wide variations in the rates charged by non-contracted ambulance service providers.
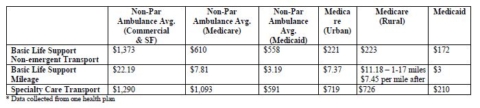
The chart below provides examples of the rates charged by non-participating ambulance service
providers compared to the rates paid by Medicare and Medicaid.
S.3526/A.6211 would require health plans to reimburse ambulance service providers regardless of
whether they are in-network or out-of-network. This creates a perverse incentive for providers to remain out-of-network, which, in turn, damages health plans’ networks. With no incentive to join plan networks, the bill would require plans to pay ambulance providers more, which ultimately would mean higher costs to consumers.
Further, the bill would establish the payment rate as the “usual and customary rate” but does not define usual and customary or who sets that rate. Payment rates for contracted ambulance providers are currently decided in a fair manner by negotiations between health plans and the ambulance company. Depending upon the health plan, non-contracted ambulance companies are paid some form of one of the following:
- the plan’s usual and customary reimbursement rate, which is typically the average rate or charge for identical or similar services in a certain geographic region;
- the average of either the rate charged by providers or the health plan’s contracted rates in that
region; or - a percentage above the Medicare rate.
If the standard for paying out-of-network non-contracted ambulance providers is set at the ambulance company’s usual and customary, this could result in health plans having to pay excessive charges. This would create an incentive for contracted providers to drop out of health plans’ networks to obtain higher reimbursement rates and establish a dangerous precedent that other providers would seek to follow.
In 2014, New York adopted one of the most comprehensive laws regarding out-of-network billing in the country. One of the law’s key elements was the creation of the Independent Dispute Resolution (IDR) process, which allows out-of-network physicians to negotiate directly with the consumer’s health plan to establish a reasonable level of reimbursement for their services, holding the consumer harmless. A more balanced approach to address this issue of out-of-network ambulance services would be to require ambulance providers to utilize the IDR process in the same manner that out-of-network physicians must follow.
For all these reasons, HPA opposes S.3526 /A.6211.
