Memorandum in Opposition |
| For Immediate Release: February 10, 2022 Re: S.1413 (Rivera) A.2383 (Niou) – AN ACT to amend the insurance law, in relation to capping cost sharing for insulin |
This legislation, S.1413/ A.2383, would require that a covered individual pay no more than $30 out of pocket for a 30-day supply of insulin medication.
While we support the goals of ensuring access to necessary, life-saving medications and access to emergency refills of these medications, the New York Health Plan Association (HPA) opposes capping the cost-sharing of insulin to $30 for a 30-day supply. While well intentioned, limiting cost sharing does nothing to improve affordability by failing to address the major driver of skyrocketing health care costs: the increasing escalation and exorbitant prices drug manufacturers charge.
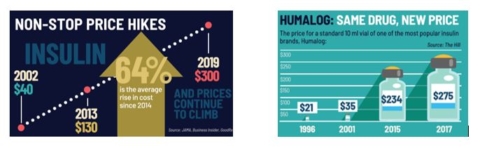
The patent for the discovery of insulin was sold to the University of Toronto for only $1 so that this lifesaving drug would be available to everyone who needed it. However, Big Pharma has repeatedly hiked insulin prices at rates far out-pacing inflation, despite little or no improvement to the life-saving drug. As the U.S. Senate Committee on Finance noted in its January 2021 bipartisan report on insulin price increases, two of the largest insulin makers in the U.S. would closely monitor the other’s prices and match or top any price increases. As the report stated, “Rather than seeking to undercut its competitors’ pricing, from 2014 on Novo Nordisk engaged in a cat-and-mouse strategy of pricing that followed Sanofi’s price increases closely, sometimes mirroring them within days or even hours.”
Even though the drug has been in use for over 100 years and no change has been made to the formula or delivery, its price has skyrocketed over the last decade, placing an even bigger burden on patients and the health care system. According to the Health Care Cost Institute, the average point-of-sale price of insulin nearly doubled from 2012 to 2016. That translates to an increase from $7.80 a day in 2012 to roughly $15 a day in 2016 for someone using an average amount of insulin (60 units per day), with the list price for a single vial of insulin costing nearly $300. As most patients use two to four vials per month, without insurance the price can become unaffordable for most individuals.
Legislation to restrict cost-sharing amounts misses the mark to keep coverage affordable for all consumers and fails to address the escalating costs of medication set by prescription drug companies. Various types of cost-containment and cost-sharing mechanisms help to control health care costs and keep monthly premiums at a minimum. Restricting or limiting cost-sharing levels increases monthly premiums and places an additional financial strain on small businesses and working families. Rather than limiting cost-sharing, the focus should be on measures to promote greater accountability into lowering their prices and making prescription medications more affordable for New Yorkers.
New York has already taken steps to contain the cost of insulin for individuals living with diabetes. The 2020 New York State Budget included a provision limiting cost sharing for insulin to $100 per 30-day, a measure supported by the American Diabetes Association. Additionally, the Affordable Care Act (ACA) includes a number of provisions concerning cost-sharing levels, making this bill unnecessary. For example, the ACA requires that health insurance products adhere to strict annual cost-sharing limits. Each individual enrollee’s out-of-pocket expenditures may not exceed a certain dollar amount every year. In accordance with the ACA, health insurance products must fit into narrow actuarial value ranges, meaning that the ratio of consumer costs to insurer costs is heavily regulated. Limiting the amount of cost-sharing for a specific benefit would significantly increase the actuarial value of a health plan, bringing it into a higher metal tier and raising the premium cost for the consumer.
Finally, this legislation would pertain only to fully-insured policies, which are purchased either by individuals who purchase coverage on their own or receive it through a small or medium-sized business. Large companies typically “self-insure,” providing employee health benefits by directly paying health care claims to providers. More than 50 percent of the commercial market is enrolled in a self-insured plan, which are governed by the federal Employee Retirement Income Security Act (ERISA) and are not subject to state mandated benefits. Included in ERISA is a provision preventing states from deeming employee health benefit plans to be in the business of insurance for the purpose of state oversight, which preempts states from regulating these plans. As a result, S.1413/ A.2383 would apply to less than half of the commercial market.
At a time when New Yorkers are grappling with the high cost of health care, legislative proposals limiting cost-sharing agreements at set amounts exacerbates this challenge and does nothing to address the spiraling underlying costs of insulin and other prescription drugs.
For these reason, HPA opposes S.1413/A.2383.
